After being badly injured in an accident, you should be able to rest and focus on your recovery. Unfortunately, you’ll likely find much of your time taken up by dealing with insurance companies and medical administrators. Dealing with insurance and medical payments is difficult regardless of your health status. After a serious auto wreck, however, it could be just too much to deal with on your own.
Even after your own insurer has paid your claim, your healthcare provider may come to you demanding additional payment. This tactic is known as balance billing. In some cases, balance billing is illegal.
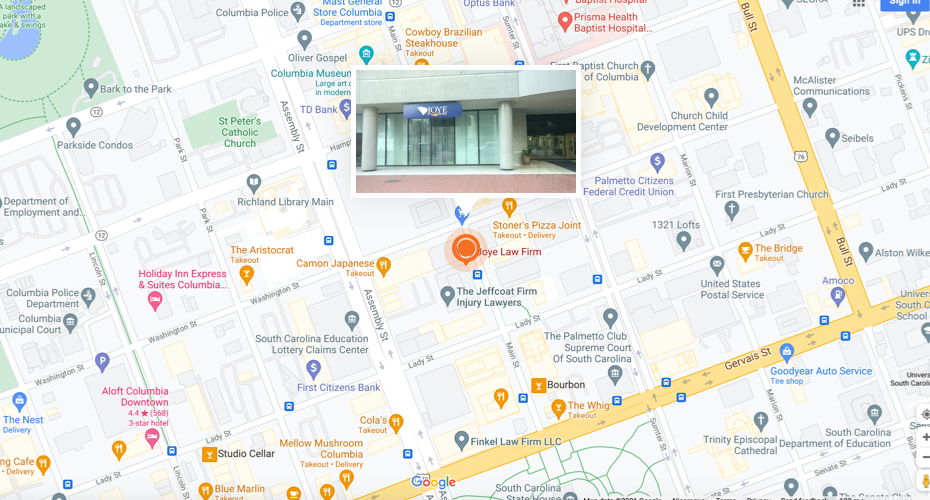
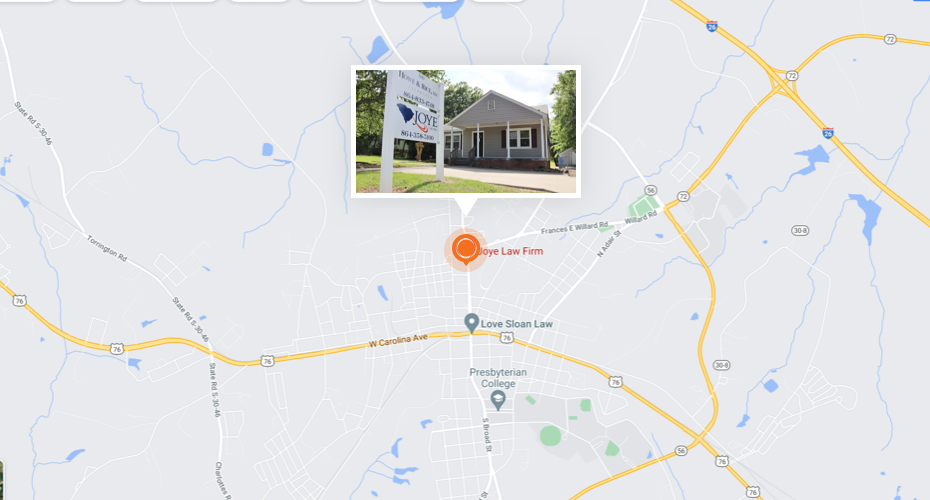
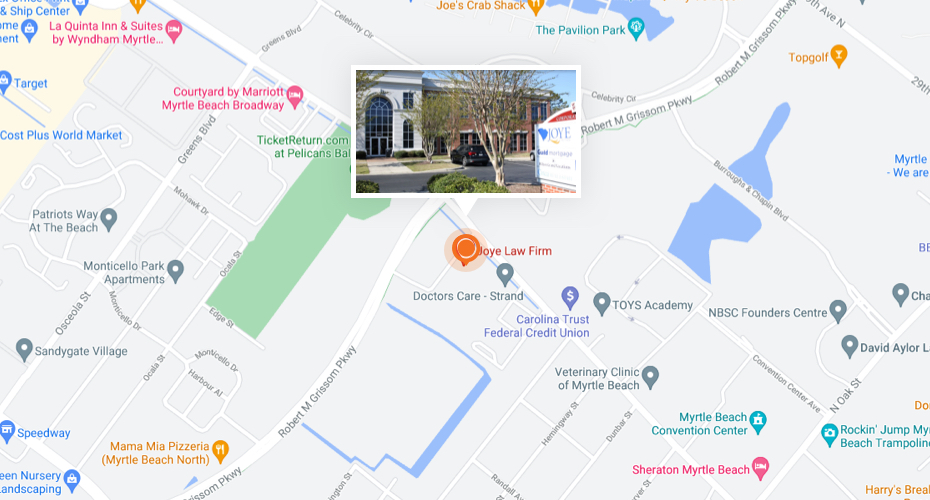
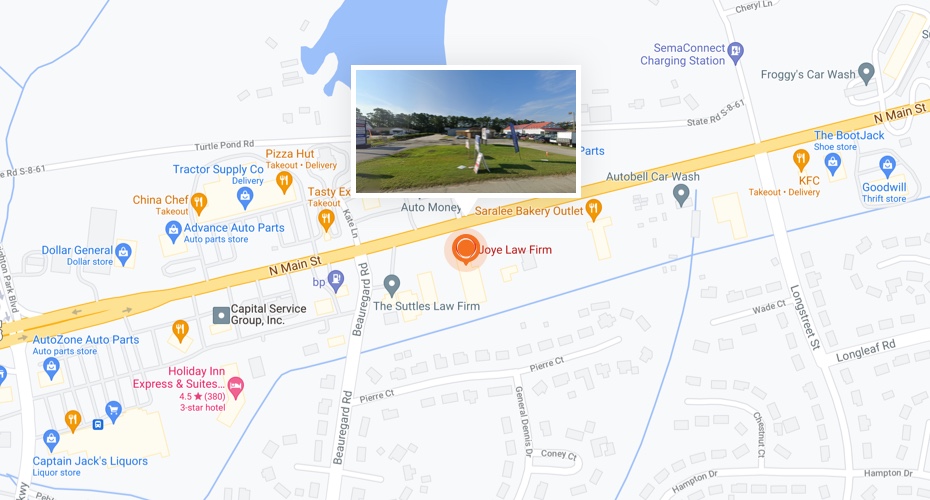
At Joye Law Firm, we believe that if doctors have a problem with their payments, they should talk with the insurance company instead of pressuring their patients.
If you or a loved one has been injured in a car crash or another accident, let our attorneys act as a buffer between you and a healthcare provider who resorts to balance billing. Our attorneys can handle your insurance claim while protecting you from aggressive billing practices. If a healthcare provider calls seeking payment, tell them to speak to your attorneys at Joye Law Firm! Contact our South Carolina personal injury attorneys today for a free consultation.
What Is Balance Billing?
Balance billing occurs when a patient is billed for the difference between a healthcare provider’s original charge and the amount the patient’s insurance has paid the provider. It often happens when a person with health insurance receives medical care from a provider or a facility outside of their health plan’s network.
Balance billing is also referred to as surprise billing because the bill is unexpected.
In a typical scenario, you are taken to the hospital for treatment after a serious accident. The hospital or individual providers then submit their requests for insurance reimbursement. Sometimes the insurance company pays 100% of the charges sought for medical services. But typically, the insurer pays a set amount of what a doctor or hospital charges.
Some providers will try to get you to pay the difference between what they charge and the amount the insurance company pays. For example, if the provider billed $1,000 and the insurer paid $750, the provider may bill you for the remaining $250.
Unless there is an agreement not to bill the balance, medical providers may bill patients for any amount not paid by most insurance.
People with Medicare, Medicaid, TRICARE, or who receive care through the Veterans Administration or Indian Health Services are not at risk for balance billing. Agreements between these programs and healthcare providers include clauses that prohibit balance billing.
Understanding Your Health Insurance Policy
Navigating the complexities of your health insurance policy can seem daunting. However, understanding key components is essential to avoiding unexpected medical bills. In this section, we will guide you through some policy basics:
In-Network vs. Out-of-Network Providers
Provider networks consist of doctors, pharmacies, and facilities that contract with insurance companies. In-network providers have agreed to provide services to members at a negotiated rate. Visiting in-network providers generally means lower out-of-pocket costs for you, as your insurance covers a larger portion of the costs.
Out-of-network providers have not agreed to the negotiated rates with your insurance company. Seeking services from out-of-network providers can result in higher out-of-pocket expenses. Insurance plans typically cover a smaller percentage of costs for out-of-network providers, if any.
Deductibles
Your deductible is the amount you must pay out-of-pocket for healthcare services before your health insurance begins to pay. For example, if your deductible is $1,000, your health insurance plan won’t pay anything toward some services until after you’ve already paid $1,000 out-of-pocket. Understanding your deductible is crucial for planning your healthcare expenses and what you may be responsible for.
Copays
Copays are fixed amounts you pay for a covered healthcare service. The amount can vary by the type of service. For instance, visiting a primary care physician may have a $20 copay, while emergency room visits could have a $100 copay. Copays generally do not count towards your deductible, but do count towards your maximum out-of-pocket costs.
Balance Billing
Balance billing occurs when a healthcare provider bills you for the difference between their charge and the allowed amount by your health plan. This is especially common with out-of-network providers. For instance, if the provider charges $1,500 for a service but your insurance only covers up to $1,000, you might be billed for the remaining $500.